Is your PBC under control?
Download Discussion Guide








.avif)
Dr. Hin Hin Ko is a gastroenterologist and clinical professor at the University of British Columbia’s Faculty of Medicine and St. Paul’s Hospital in Vancouver, BC.
PBC is an autoimmune condition in which the immune system mistakenly attacks bile ducts in the liver. Because their immune systems are overactive, patients with PBC are more prone to other autoimmune conditions, such as thyroid disease. This is something that we screen and regularly check for.
Higher cholesterol levels are common amongst patients with PBC as well. Interestingly, studies have shown that despite elevated cholesterol levels, patients with PBC do not have an increased risk of complications like heart attack or stroke.
No — there seems to be no direct correlation in PBC between one’s symptoms (i.e. fatigue, pruritus) and the severity of the liver damage. This is good news because while some people can feel quite tired and itchy, their blood work looks fine, indicating that PBC is under control. On the other hand, we also have some patients with severe liver disease who do not experience any symptoms.
Blood tests are crucial for monitoring disease progression, and what we’re usually keeping an eye is alkaline phosphatase. We monitor the liver function too, for example checking the bilirubin. We also recommend doing bone density scans every few years, and monitoring vitamin D and cholesterol levels about once a year.
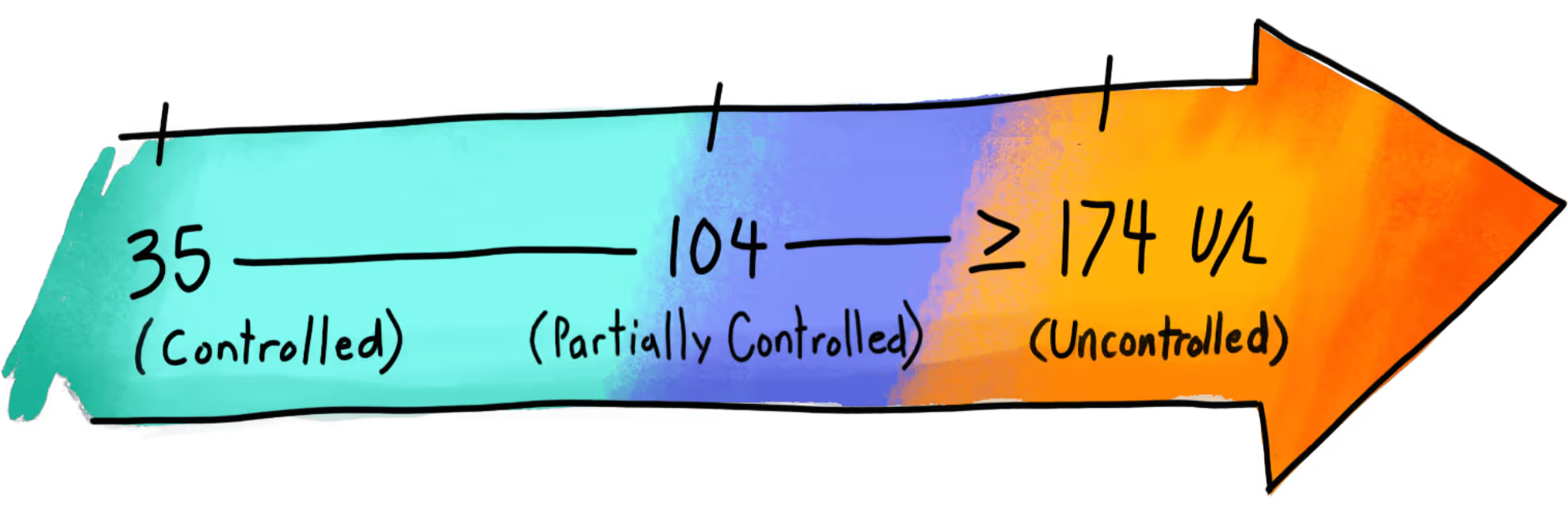
ALP is an enzyme that we monitor to check how well the bile ducts are functioning and whether PBC is under control. In people with PBC, high ALP levels usually mean there’s ongoing inflammation and damage to the bile ducts within the liver, which leads to toxic bile accumulating in the liver. With effective treatment, we want to see ALP levels coming down from the baseline and ideally staying below 200 IU/L — that’s a sign of a good treatment response and a much lower risk of developing liver scarring (fibrosis), cirrhosis, or needing a transplant.
When starting treatment, I typically recommend checking ALP levels every three months to make sure we’re heading in the right direction. If the numbers are consistently good, we can reduce testing to about twice a year.
If your ALP levels aren’t improving and remain elevated, that means your PBC isn’t under adequate control with the current treatment. It also means there’s some ongoing inflammation of the bile ducts within the liver, which can cause scar tissue and eventually put you more at risk of developing cirrhosis and complications from the cirrhosis.
The most important thing you can do is to stay in close follow-up with your specialist to ensure that your PBC is well-controlled. In addition, a healthy lifestyle can make a big difference — things like eating a balanced diet (low in fat and sugar, with plenty of fruits and vegetables), exercising regularly, limiting alcohol, avoiding smoking, and staying up to date on vaccinations (like hepatitis A and B) all support liver health.
I generally advise against liver cleanses and liver supplements, as they can potentially do more harm than good. Multivitamins are safe to take — especially since people with PBC tend to be lower in fat-soluble vitamins (A, D, E, and K). I usually recommend checking those levels and supplementing if needed. Vitamin D, in particular, is often beneficial, especially for those who don’t consume much dairy and those of us living in North America, where we don’t get a lot of sunlight, and for women over 50, who may be at increased risk of osteoporosis.
These are common concerns, but if PBC is diagnosed promptly, treated early, and monitored adequately, the answer is no. We don’t expect patients to develop cirrhosis, need a transplant, or have a shorter life expectancy if their disease is well-managed. That being said, it’s very important to stay on top of your blood work and follow-up appointments to mitigate these risks, even if you’ve had a good initial response to treatment.
Yes. Because PBC is a chronic autoimmune condition with no known cure, long-term treatment is essential. Stopping treatment can cause your liver enzyme levels to rise again, which may lead to ongoing inflammation and damage. It’s very important for patients with PBC to take their medication every single day, maintain a healthy lifestyle, and stick with regular follow-ups to keep the disease under control and reduce the risk of complications like cirrhosis. The regular checkups are especially important since symptoms do not correlate with disease control.
PBC is polygenetic, which means that multiple genes contribute to its development, with environmental factors and lifestyle choices likely also playing a role in triggering or influencing the course of the disease. Since other family members might have the genetic predispositions, it’s a good idea to make them aware of your condition so they can be monitored for potential risk factors, such as through liver enzyme blood work, at their next annual checkup. This is especially important if you have a daughter or sister, as PBC is a female-predominant condition.

