Whether you’ve recently been diagnosed with kidney disease, or have been living with it for a while, there are always new things you can learn to help support your health.
Let’s start with the basics.
The kidneys are two bean-shaped organs that are important for filtering waste products from the blood. They also play a role in managing blood pressure, keeping our bones strong, and producing red blood cells.
Chronic kidney disease (CKD) is a progressive disease, which means that it doesn’t occur overnight, but develops over time — typically over three months or longer. There are five stages of CKD and they’re measured based on your estimated glomerular filtration rate (eGFR), which is the percentage of your remaining kidney function. CKD can result from kidney damage created by other diseases like diabetes or high blood pressure, or from genetic or autoimmune disorders. Understanding the cause of your kidney disease can help you manage your kidney function.
What happens with kidney disease?
The term “chronic” in CKD means that damage to the kidney filtering units has occurred over a period of time.
As kidney function declines, waste products in the blood begin to accumulate and other symptoms arise. This might include a decrease in appetite, fatigue or tiredness, swelling (edema), shortness of breath, decreased mental sharpness or difficulty concentrating, urinating less frequently, changes in urine colour (it may be foamy, dark orange, brown, or tea-coloured), sleep problems, and muscle cramps or restless legs. These symptoms all occur because of the buildup of waste products in the body.
Managing kidney disease
With CKD, your kidney function will slowly decline over time. While CKD isn’t reversible, the progression of the disease, or the damage, can be delayed. Here are some strategies for managing CKD:
Check in with your health care team
Regular follow-up appointments with your health care team are important. Your family doctor may be monitoring your function, or at later stages you may be referred to a nephrologist (a doctor who specializes in treating kidney disease) for more support. They are able to check your kidney function using blood and urine tests, which helps them to keep an eye on the progression. It’s also important to discuss any health or medication changes with your health care team so that they can adjust your treatment plan accordingly.
Stay as healthy as possible
Nutrition
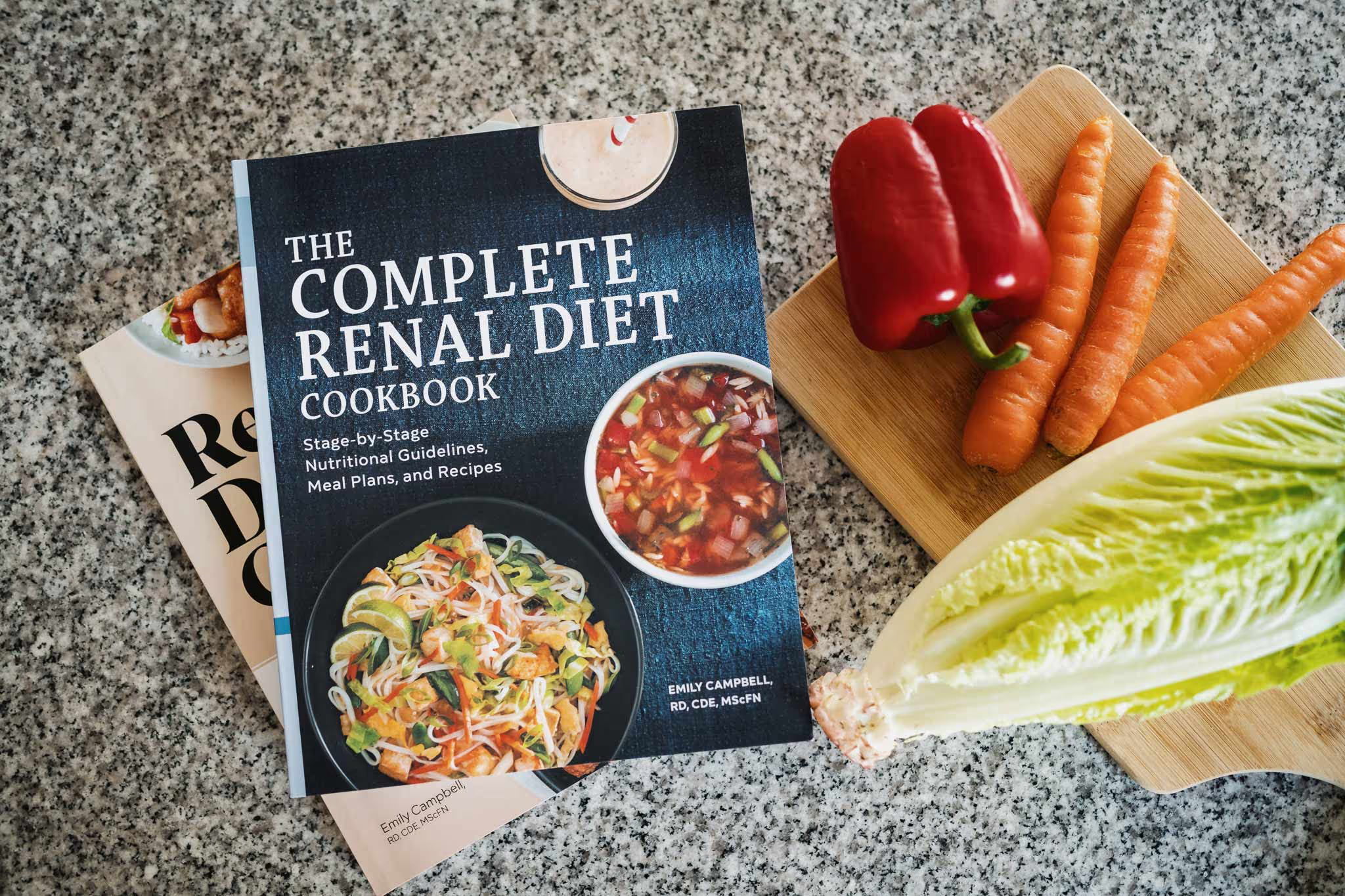
Optimizing nutrition is an effective strategy for helping to delay the progression of CKD. Proper nutrition can help to minimize waste products from building up in the blood. When you make the right nutritional changes and diet choices, then the kidneys will have less waste to filter, and their function can be preserved. The foods we choose can also help to manage your blood sugar and blood pressure values, which can cause damage to the kidneys when uncontrolled. Finally, maintaining proper nutrition help to stabilize lab values for electrolytes (like potassium or phosphorus) at later stages of disease progression.

Understanding your stage of kidney disease helps empower you to ask your health care team questions and to make the right changes to your nutrition. Work with a registered dietitian who can provide personalized recommendations to manage your CKD through a proper food plan. Here are some strategies to help get you started:
- Reduce sodium to help manage blood pressure and ease kidney filtration.
- Aim for a balanced plate at each meal by including lots of vegetables (aim for half your plate), a quarter of your plate of carbohydrates or starches (like bread, pasta, or rice), and a quarter of your plate (or a palm-sized portion) of protein (especially more plant-based proteins) to help ensure you get enough of the right nutrients. You may need to make changes to the types of foods you’re eating depending on the potassium or phosphorus values in your blood.
- Make water your beverage of choice, and avoid juice and pop as they typically just add calories and have limited nutritional value.
Physical activity
Physical activity is important for people with CKD because decreased kidney function can affect your muscles and bones. When your kidney function decreases, it can make you feel tired or weak and can cause joint pain. Physical activity can help increase your energy levels, improve blood pressure and stress levels, and reduce restless leg symptoms.
It’s safe to participate in physical activity like walking, biking, light resistance training, and flexibility and balance exercises with CKD. However, it’s important that you speak with your health care team before starting a new routine.
Manage other health conditions
Diabetes, high blood pressure, and high cholesterol are associated with CKD. It’s important to take medications as prescribed and to work to keep your blood sugar, cholesterol, and blood pressure at target as this helps to preserve kidney function.
Become your own expert
CKD may lead to some changes in your life, but it doesn’t define who you are. Taking control of your CKD and becoming your own expert can help you manage your condition. Start with these tips and tricks:
- Learn about your condition.
- Join support groups.
- Understand what your blood and urine results are and what they mean.
- Ask your health care team questions. Write them down before your appointment and take them with you. For example:
- What is my eGFR? Has it changed since my last appointment?
- What can I do to keep my disease from getting worse?
- Do I need to change what I eat? Is a dietitian available?
- What supports are available for me and my loved ones to learn about my disease?
- What happens next?
You’re not alone on this journey. Speaking with others who are living with CKD and getting answers about CKD is important. Connecting with organizations like the Kidney Foundation of Canada can help you navigate what living with kidney disease may mean for you, and provide you with further resources and emotional and financial supports.
Emily Campbell (@kidneynutrition), RD, CDE, MScFN, is a registered dietitian, certified diabetes educator, cookbook author, and the founder of kidneynutrition.ca. Emily specializes in renal nutrition, helping those with chronic kidney disease overcome the confusing world of nutrition.