Cutaneous T-cell lymphomas (CTCLs) are a rare group of non-Hodgkin lymphomas, which are forms of blood cancer. The most common subtype of CTCL is Mycosis Fungoides (MF) — a slow-growing lymphoma whose first signs and symptoms typically include small patches and plaques on the skin. Because these lesions are often mistaken for other more common skin conditions, such as psoriasis or eczema, MF can be difficult to diagnose. Sézary Syndrome is a more rare and aggressive form of CTCL that affects the skin, but which also affects the blood and lymph nodes and can spread to other organs.
Patient Voice connected with Dr. Robert Gniadecki, a dermatologist at the University of Alberta, and Dr. Gizelle Popradi, a hematologist who treats malignant blood disorders at the McGill University Health Centre, to learn more about diagnosing CTCL, treatment options, and more.
Please note: the information contained in the following responses is based on the research and clinical experiences of the interviewees and does not necessarily represent the views or opinions of the publisher or associated sponsor.
What are the key signs and symptoms that might suggest a patient has CTCL?
Dr. Robert Gniadecki: CTCL isn’t just one disease — it’s a whole family of diseases where T lymphocytes, a type of immune cell, grow uncontrollably in the skin.
The most common form, Mycosis Fungoides (MF), often starts with a red, itchy rash that can look like eczema or psoriasis. It typically appears on areas that don’t get much sun, like the trunk, buttocks, or inner thighs. Some CTCLs are more aggressive and start as nodules or tumours, but that’s much rarer. In the early stages, it’s very subtle — so subtle that even dermatologists can have difficulty diagnosing it. This diagnostic challenge means that some patients can live with CTCL for years before it’s accurately identified and treated.
A red flag that I look for is when a rash doesn’t improve — or worsens — with initial treatment. That’s typically when a family doctor will refer a patient to a dermatologist like myself.

Dr. Gizelle Popradi: CTCLs are an uncommon group of lymphomas and therefore a rare cause of skin disease. This makes their diagnosis challenging for doctors. We’re still learning about the biology of CTCL, but the reason that CTCL appears on the skin likely has to do with the uncontrolled growth of white blood cells, called memory T-cells, that are involved in the disease’s development. In advanced cases, CTCL can also spread through the blood to affect lymph nodes and internal organs.
Download the CTCL discussion guide.
What tests can help diagnose and stage CTCL, and what information do these tests provide?
Dr. Gniadecki: When a patient is referred to a dermatologist, we may recognize CTCL based on its appearance, or we may need to order a biopsy. Biopsies are the only way to confirm CTCL in the early stages. But even with a biopsy, the diagnosis isn’t always clear — we sometimes need multiple biopsies to catch the abnormal cells that help us diagnose CTCL.
In early-stage disease, imaging and blood tests usually don’t show anything abnormal because the lymphoma is still confined to the skin. There’s nothing to find in the organs or lymph nodes, and no signs of disease in the blood. But if CTCL has progressed to tumours, which we call stage 2, then we can use PET scans, lymph node biopsies, and specialized blood work to see if the cancer has spread beyond the blood into the lymph nodes and internal organs.
Dr. Popradi: Making the diagnosis of CTCL is challenging. Skin biopsies may be helpful in patients without erythroderma (full body redness and inflammation), but even when the disease is limited to the skin many biopsies may be necessary to secure a CTCL diagnosis, done in conjunction with a patient’s history of typical persistent patches and plaques in non-sun-exposed skin areas. It’s important to remember that making links between the clinical history of the patient and the biopsy results are often necessary to secure a confident diagnosis.
.avif)
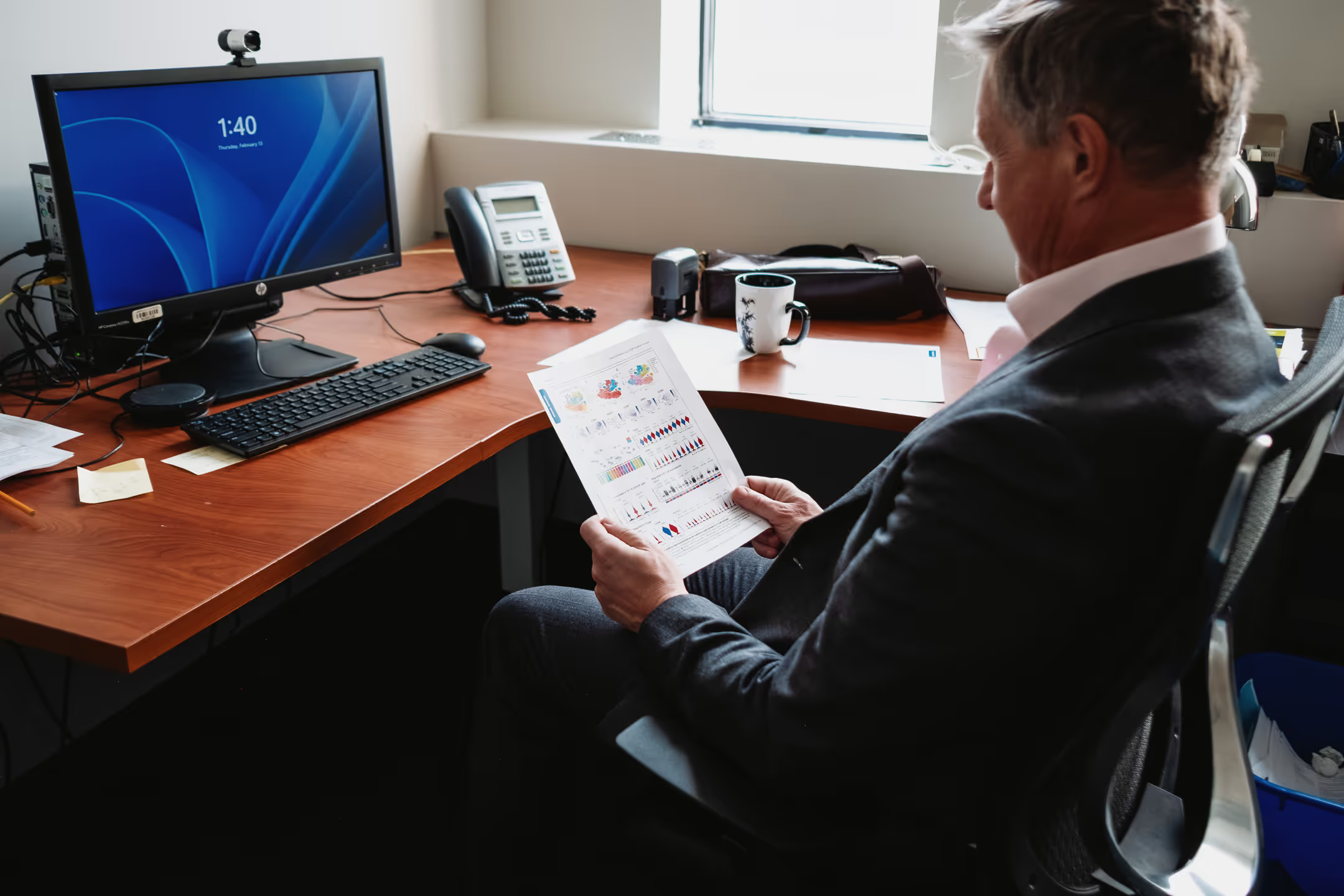
How do dermatologists and hematologists work together to ensure the best outcomes for CTCL patients?
Dr. Gniadecki: CTCL is a disease that affects both the skin and the blood, so collaboration between dermatologists and hematologists is key. In early-stage CTCL, the dermatologist plays the biggest role in identifying and treating the symptoms. If the disease progresses, then we work closely with hematologists and oncologists to design a holistic treatment plan for the patient. But whenever we can, we have hematologists and oncologists see patients quite early, as it makes following the patient easier if the disease advances. And even if a patient moves into hematologic care — typically because their disease has progressed beyond the skin and is now affecting the blood, lymph nodes, or internal organs — dermatologists remain involved because the skin symptoms — itching, wounds, infections — are often the biggest quality-of-life concern.
Dr. Popradi: At the multidisciplinary clinics I work at, dermatologists, hematologists, radiation oncologists, and pathologists all work together to manage and diagnose CTCL. Having multiple specialists involved from the beginning of a patient’s journey ensures a more comprehensive approach to care — whether it’s managing skin symptoms, staging the disease, or deciding on a multipronged treatment plan. A multidisciplinary approach is essential because it ensures that we’re taking care of the many aspects of CTCL that affect a patient’s health and quality of life.
Download the CTCL discussion guide.
What are the treatment options for CTCL, and how do they vary based on the stage of the disease?
Dr. Gniadecki: For early-stage CTCL, treatment is focused on the skin — medications and phototherapy are used. Total body radiation is another treatment option, but access can be a challenge — it’s only available at two centres in Canada. While waiting to see a doctor, patients can take steps to manage their symptoms. Moisturizing regularly and taking bleach baths (by adding a small amount of bleach to bathwater) to reduce bacteria and prevent infection can help.
A lot of patients can struggle with sleep because of their skin’s itchiness. Stress can make the itch worse, creating a vicious cycle. Anything that helps manage stress — good sleep hygiene, relaxation techniques — can help break that cycle.
We often talk to patients about general health habits that can improve their outcomes. Things like eating whole, unprocessed foods, cutting down on refined sugars, maintaining a healthy weight, and staying as active as possible can all be beneficial. Healthy lifestyle modifications are super important and easily overlooked.
Dr. Popradi: Treatment options are varied and really depend on the stage of the disease. Dermatologists typically guide care in early stages of CTCL and commonly use skin-directed therapies to control symptoms. However, for more advanced CTCL, such as forms that present with tumours and erythroderma, hematologist-oncologists are often involved. With advanced stages of disease, or disease that doesn’t respond to skin-directed therapy, we typically turn to oral therapies. We may also use extracorporeal photopheresis (a blood-filtering treatment), intravenous immunotherapies, or chemotherapies, sometimes in combination with radiation therapy. In certain rare cases, allogeneic stem cell transplantation may be recommended. We tend to layer on therapies, gradually increasing the intensity to achieve the best results with the least toxicity. Therapy is always guided by the goals of care, consideration of a patient’s quality of life, and the stage of the disease.
The treatments mentioned above may not be suitable for everyone and may cause side effects. Consult a health care professional for complete information on the condition and available treatment options.
What advice would you give to someone who suspects they might have CTCL, and how can they advocate for themselves to expedite diagnosis and treatment?
Dr. Gniadecki: If a rash or skin condition doesn’t respond to treatment, I’d encourage patients to feel comfortable asking their doctor to reconsider the diagnosis, or seek a second opinion from a dermatologist with experience in CTCL.
Dr. Popradi: It’s important to remember that CTCL is extremely rare, so if you’re experiencing a persistent rash, there could be a number of different causes. That being said, if a rash doesn’t improve with treatment, it’s reasonable to ask your doctor for a skin biopsy. If the results still aren’t clear, ask if they should be reviewed by a pathologist with expertise in cutaneous lymphomas, or ask for a referral to a CTCL specialist.

It’s always important for patients to advocate for themselves. If you’re diagnosed with CTCL, remember that you’re not alone. Most patients with early-stage CTCL go on to live fulfilling lives. This disease is different from other cancers in that it often progresses very slowly — there’s time to investigate, confirm the diagnosis, and determine the best course of action.
Download the CTCL discussion guide to help speed up the conversation with your physician about testing and specialized care.
This article was created by Patient Voice on behalf of Kyowa Kirin Canada Inc.

.jpg)