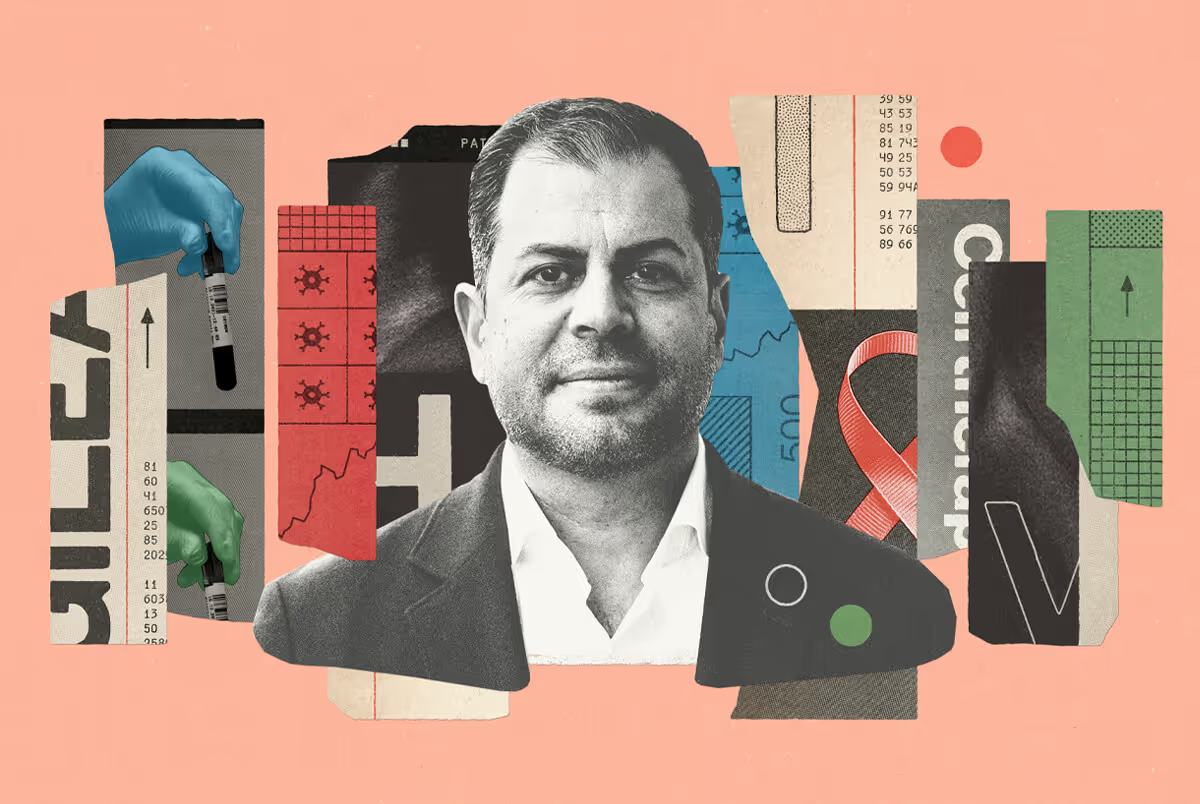
Dr. Dodig is a neuromuscular neurologist with the University Health Network, University of Toronto, and William Osler Health Centre.
1. What is gMG and how does it present?
gMG is a chronic autoimmune, neuromuscular disease that mainly manifests as muscle weakness. The weakness may affect ocular (eye) muscles, cervical (neck) muscles, bulbar (mouth and throat) muscles, respiratory muscles, and the limbs. Depending on the muscles affected, this can present as double vision, droopiness of the eyelids, speech difficulties, swallowing or chewing problems, weakness of the upper or lower extremities, abnormal breathing patterns, or blunted ventilatory responses.
What’s striking about the muscle weakness associated with gMG is that it’s fatigable — someone may have full strength at first but as they exert themselves, the muscle becomes weaker. Patients’ symptoms can therefore fluctuate. As such, gMG has been called “the great mimicker” and it’s difficult to recognize. It’s also sometimes associated with a tumour of the thymus, so it’s important to exclude any associations with thymoma.
“Because gMG can be difficult to recognize, it often takes years to receive an accurate diagnosis.”
2. How is gMG diagnosed? How long does it typically take to receive an accurate diagnosis?
To diagnose gMG, we rely heavily on patients’ histories. As doctors, we must be extremely attentive listeners so we can fully understand patients’ symptoms. We also rely on clinical examination, although since the weakness is fatigable and we’re just taking a snapshot in time during the exam, patients may not always exhibit obvious signs of weakness. Sometimes we exercise the muscle to induce the weakness, such as droopiness of the eyelids or double vision, for a more reliable examination.
We also use supporting tests for diagnosis, including electrodiagnostic testing and blood work. With electrodiagnostic testing, we test individual nerves by stimulating them with an electrical impulse, and then we record the response in the muscle. If there’s any impairment at the neuromuscular junction, you can actually see the decrement in the response. However, there’s a significant subset of patients who have normal repetitive nerve testing, so we also use a test called single-fibre EMG, in which we measure the time for the signal to be transmitted to the nerve ending. Because gMG can be difficult to recognize, it often takes years to receive an accurate diagnosis.
3. How is the complement system involved in gMG?
There’s a whole cascade of immunological events that occurs as a result of the presence of the antibodies in gMG, and one very important part of it is complement. The anti-acetylcholine antibodies are primarily immunoglobulin IgG1 or IgG3, which contribute to complement activation. Complement activation results in a series of physiological processes that culminate in the muscle not being able to respond to the nerve endings’ triggers, making it unable to contract and therefore weaken.

4. Why is it important to protect the neuromuscular junction?
The neuromuscular junction is where nerves and muscle fibres meet. This junction allows nerves to communicate and trigger muscle firing, so if there’s any impairment in transmission across the neuromuscular junction, then muscle weakness is the result. Through a cascade of mechanisms that leads to activation of the complement, known as complement-mediated membrane destruction, you end up losing the normal structure of the neuromuscular junction. It’s important to recognize and treat gMG early to prevent this damage and the subsequent muscle weakness.
From a physician perspective, we’re primarily concerned about life-threatening symptoms such as breathing and swallowing difficulties. But gMG affects patients in many ways and on many levels — impacting their physical, social, and emotional well-being. Their day-to-day functioning may be affected, including their ability to drive, cook, pursue hobbies, participate in sports, and socialize.
In addition to the physical and social impacts, there’s also a significant emotional impact that comes with this type of condition — patients often experience anxiety, fear, depression, frustration, and shame. gMG can also impact sleep and obviously if one’s work is affected, that can lead to financial difficulties.
5. What does a typical treatment journey look like for someone living with gMG?
There has been a great expansion of gMG research and literature over the years. Our ability to manage gMG has improved significantly, as has the mortality rate for gMG patients.
Currently, we use a combination of therapies to manage gMG depending on the subtype and the patient’s characteristics. For example, different therapies may be selected based on a patient’s antibody status, whether symptoms are primarily ocular or generalized, whether or not they have thymoma, the age of onset, the severity of disease, and their gender and childbearing status. We also have to account for other comorbidities that may limit or complicate the therapies.
Finally, it’s crucial to recognize patients’ preferences, because we need to have a solid patient-physician rapport in order to navigate the ups and downs of this condition. Fortunately, there are many new therapies coming onto market, yet patient access is limited. We’re discovering more and more information about these therapies and are hopeful that we’ll continue to see innovation in this space in the years ahead.
Neuromuscular disorders like myasthenia gravis are often misdiagnosed or diagnosed late, but Muscular Dystrophy Canada (MDC) is working to ensure Canadians can get an early and accurate diagnosis to receive the right resources, treatments, and therapies. Currently, MDC is learning about the diagnostic and treatment experiences of Canadians affected by myasthenia gravis. If you or someone you know is affected by myasthenia gravis, and would like to participate in this Journey Mapping study, email research@muscle.ca or call 1-800-567-2873 ext. 1114. For more information visit this link.
This initiative was supported by Alexion AstraZeneca Rare Disease. The content was developed by Patient Voice, and the supporter did not influence the final article or editorial themes.
%20(1).jpg)